PCOS & Infertility: How Jenny overcame her PCOS diagnosis and became pregnant
A 36 year old nurse, Jenny came to our clinic after trying to get pregnant for the past year. Her story was a familiar one. She had been on the pill for nearly a decade to help ease and manage her periods. When she and her husband were ready to grow their family, she came off the pill and figured they’d get pregnant within 3-4 months.
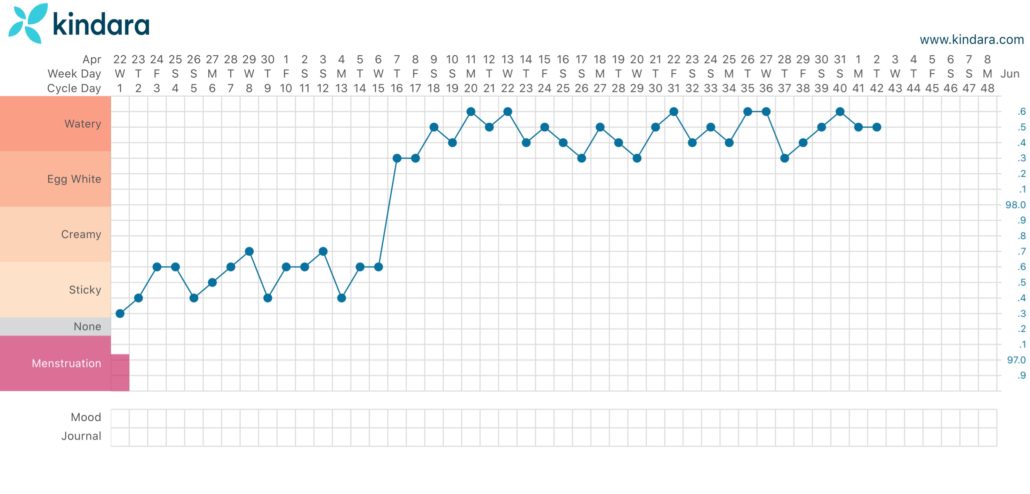
Very quickly though, she began to notice some red flags. Her cycles were irregular and long (ranging from 40-60 days) and her ovulation predictor tests never came up positive.
6 months later and still not pregnant, she went to her Obgyn, who after some bloodwork told Jenny that she had polycystic ovarian syndrome (PCOS).
The two main characteristic of PCOS are high androgen levels (high levels of male hormones) and anovulatory cycles (cycles where you’re not ovulating).
PCOS & Coming off the Pill
Jenny fit the bill on both ends, but it seemed like her case might be temporary post-pill pcos. It is typical for some people to experience a rise in male hormones along with irregular cycles after being on the pill. Often times this will get resolved with time, but in some instances, the symptoms can persist for months.
It was a frustrating diagnosis, feeling like her body was ‘broken,’ unable to do something that it normally used to do. To top it all off, she felt like she wasn’t getting any younger and that she was running out of time.
Her Obgyn’s approach was to stimulate ovulation using a drug called clomid and to do an IUI. She went through three rounds of clomid + IUI but still no pregnancy.
Solving the PCOS Puzzle
Jenny was referred to our clinic through a friend who had good success with their women’s health issues at our clinic. She knew we specialized in fertility and was looking for answers.
Her first acupuncture session was less about the acupuncture and more about gaining an understanding of what was going on with her body and catching on to its clues. We went over her cycles: what sort of symptoms she experienced pre-menstrually and on her period – and what it all meant in terms of her hormone health.
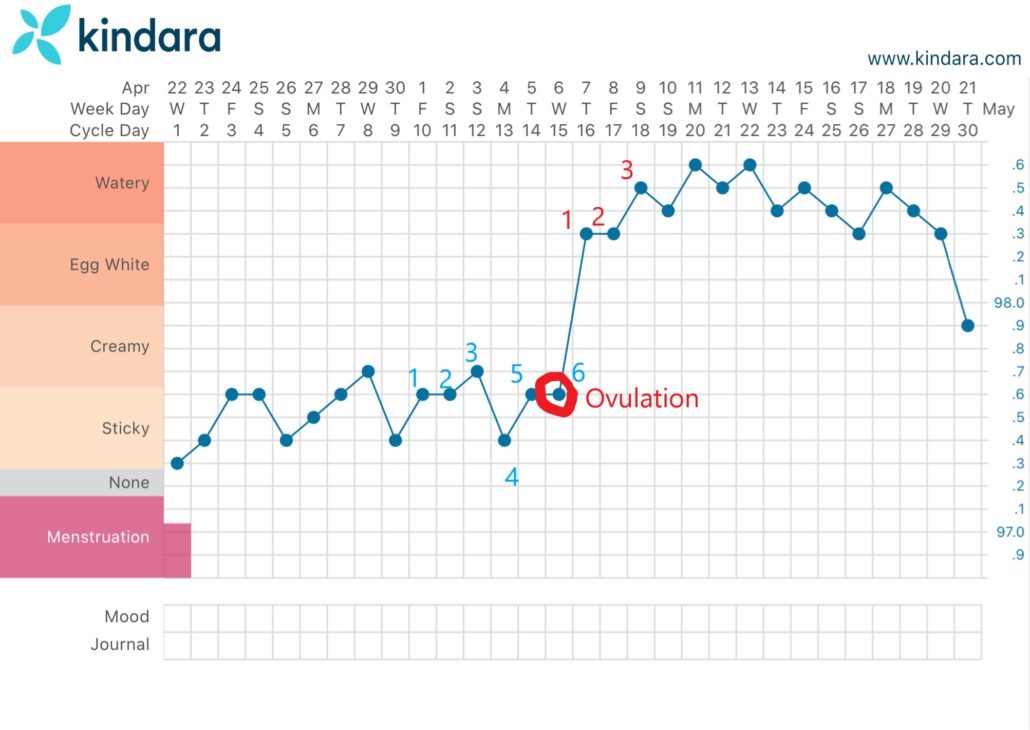
She was put on a weekly acupuncture + supplement regimen and by the 3rd month her body began to ovulate on its own – without the help of clomid. What’s more is that as her menstrual cycle’s rhythm was beginning to restore itself, her cycles became shorter and more in the ‘normal range.’ Her mood swings, period aches and pains all became drastically less.
Fast forward to 4.5 months from her first acupuncture treatment, Jenny found out she was pregnant!
The following are Jenny’s top 2 takeaways that helped her overcome her PCOS diagnosis and achieve a healthy pregnancy:
- Take the time to learn about the difference phases of your menstrual cycle. Understanding the different phases made it easier to look out for signs of ovulation. For people with irregular/long cycles, it can be difficult to pinpoint the 5-day fertile window during which to try.
- Just because you’re not ovulating right now, doesn’t mean your body can’t do it in the future. Your body can recover and restore its natural cycles.
If you are interested in learning more about how you can overcome your PCOS, come meet us in person/online and learn more. Your initial consultation is free: click here to request your free initial consult.